視網膜是內襯在眼球後壁的感覺組織層,感受光影與色彩,好像照相機的底片一樣 ( retina is a thin layer of light sensitive tissue on the back wall of the eye. The optical system of the eye focuses light on the retina much like light is focused on the film in a camera ) ,我們平常所稱的視網膜是指感覺層視網膜,它正常時是與視網膜色素上皮緊密黏貼,這兩層組織大部分靠脈絡膜供給其營養。
視網膜剝離 (retinal detachment) 屬眼科急症之一, 是視網膜的神經感覺層 (sensory retina) 與色素上皮層 (pigment epithelium) 之間被積液所分開 ( retina peels away from its underlying layer of support tissue ) ,感覺層視網膜就會失去營養供應而發生功能退化。其發生率約 1/20,000 ,在中老年齡 ( middle-aged or elderly population ) 發生率更高達 1/5,000 ,一般人罹患風險 ( lifetime risk ) 是 1/300 。在病初,患者眼睛會感到閃光 (flushing light) 及漂浮物 (floaters) 症狀 ,若未及時治療,視網膜完全剝離後,出現視野缺損 ( vision loss ) ,甚至失明的危險 ( Initial detachment may be localized, but without rapid treatment the entire retina may detach, leading to vision loss and blindness. It is a medical emergency) 。
一般正常人視網膜剝離的發生率約 1/20,000 ,中老年人 ( middle-aged or elderly population ) 發生率更高達 1/5,000 。一般人罹患風險 ( lifetime risk ) 是 1/300( The risk of retinal detachment in otherwise normal eyes is around 5 in 100,000 per year. Detachment is more frequent in the middle-aged or elderly population with rates of around 20 in 100,000 per year. The lifetime risk in normal individuals is about 1 in 300) 。 裂孔性視網膜剝離之病患中有 40~60 %是近視眼者 ,然而,高度近視 ( severe myopia , above 5~6 diopters) 患者罹患視網膜剝離的罹患風險上升至 1/20 。白內障手術摘除水晶體患者罹患視網膜剝離的頻率也增加了,其預估風險是 5/1,000~16/1,000 ;視網膜剝離常發生在單眼,但 15% 患者累及雙眼,合併白內障者,造成雙眼視網膜剝離風險增加至 25~30%( Retinal detachment can occur more frequently after surgery for cataracts. The estimated risk of retinal detachment after cataract surgery is 5 to 16 per 1000 cataract operations . Although retinal detachment usually occurs in one eye, there is a 15% chance of developing it in the other eye, and this risk increases to 25~30% in patients who have had cataracts extracted from both eyes) 。
發生視網膜剝離的危險因素有: (1) 既往曾經有過視網膜剝離患者 ( have previously experienced a detachment ) ; (2) 高度近視 ( severe myopia ) ; (3) 視網膜剝離家族史者 ( a family history of retinal detachments ) ; (4) 曾白內障手術 ( Cataract surgery ) :白內障手術之後,常由於玻璃體液化而發生牽引現象,睫狀肌所分泌的房水經由裂孔進入視網膜下方 (subretinal space) 而造成視網膜剝離; (5) 曾經眼球或頭部受過 ( injury or trauma to the eye or head ) 劇烈撞擊; (6) 眼內炎症者,如葡萄膜炎、 後鞏膜 炎 ; (7) 周邊視網膜之柵狀變性 (lattice degeneratian) ; (8) 瀰漫性脈絡膜視網膜萎縮 ( diffuse chorioretinal atrophy) ; (9) 玻璃體變性和玻璃體剝離 (PVD) 。
根據發生原因,視網膜剝離可分成三種,即裂孔性視網膜剝離 ( Rhegmatogenous retinal detachment , RRD) 、滲出性視網膜剝離 ( secondary retinal detachment or exudative retial detachment , ERD) 、牽引性視網膜剝離 (traction retinal detachment , TRD) 。
- 裂孔性視網膜剝離 ( 又稱原發性 ) : 視網膜破孔有 3 種形式 (types) ,即 孔 (holes) 、裂孔 (break or tears) and 離斷 (dialyses) , 80% 以上裂孔發生在周邊部。萎縮性孔 (atrophic hole) 由內層視網膜發生病態的格子狀變性 (lattic degeneration) ,使其萎縮形成的小圓孔 ( Holes form due to retinal atrophy especially within an area of lattice degeneration ) ;牽拉性裂孔是玻璃體對視網膜的牽拉所造成的 ( Tears are due to vitreoretinal traction ) ,可形成馬蹄形孔 (horse-shoe break) 或巨大裂孔 (giant tear) ;發生在周邊鋸齒緣的裂孔稱作鋸齒緣離斷 (dialyses) 。偶而, 少數後玻璃體分離 (PVD) 患者也會出現 hole 、 break 情況 ( Occasionally, posterior vitreous detachment, injury or trauma to the eye or head may cause a small tear in the retina. The tear allows vitreous fluid to seep through it under the retina, and peel it away like a bubble in wallpaper) 。 若破孔 不加以治療,玻璃體液化後,液體進入裂孔 → 視網膜下腔,使 視網膜的感覺層與色素上皮分離, 演變成視網膜剝離 ( A rhegmatogenous retinal detachment occurs due to a break in the retina that allows fluid to pass from the vitreous space into the subretinal space between the sensory retina and the retinal pigment epithelium ) 。 患者中有 40 %是近視眼者,尤其是 500~900 度之間的近視患者最容易發生 ( 因為 1000 度以上之近視比較容易出現黃斑部附近的脈絡膜及色素層的萎縮,但黃斑部萎縮到一個程度也可能出現裂孔 (macalan hole)) 。
- 滲出性視網膜剝離 ( 又稱繼發性 ) :多見於葡萄膜炎、後鞏膜炎、受傷、血管異常如視網膜血管瘤、脈絡膜黑色素瘤 ( choroidal melanoma ) ,導致 血液中液體所形成的漿液滲漏到視網膜下所致 ( An exudative retinal detachment occurs due to inflammation, injury or vascular abnormalities that results in fluid accumulating underneath the retina without the presence of a hole, tear, or break) 。
- 牽引性視網膜剝離: 因視網膜缺血引起新生血管膜的牽拉、眼球穿通傷引起纖維組織增生的牽拉等原因引起視網膜剝離 ( A tractional retinal detachment occurs when fibrous or fibrovascular tissue, caused by an injury, inflammation or neovascularization, pulls the sensory retina from the retinal pigment epithelium) 。另外在糖尿病視網膜病變或鐮刀型貧血所致的增殖性視網膜病變也可發生 視網膜剝離 ( Tractional retinal detachments can also occur in patients with proliferative diabetic retinopathy [ or those with proliferative retinopathy of sickle cell disease) 。
(註)良性周邊視網膜退變 (degeneration) 不會出現視網膜破孔,包括微細囊狀變性 (microcystoid) 、雪花狀變性 (snowflakes) 、網狀變性 (honeycomb) 、大理石狀變性 (pavingstone) 、膠狀體變性 (drusen) 、齒狀變性 (oral) ; 病態周邊視網膜退變,如格子狀變性(lattic)、蝸牛痕變性(snailtrait),有 18% 患者可以合併視網膜萎縮性孔 (atrophic hole) ,容易造成視網膜剝離。
視網膜剝離範圍可以緩慢擴大,也可在短時間內迅速進展,緩慢 發生時不痛不癢,但可以出現 3 個主要的前驅症狀:
- 突然視力模糊 ( Sudden blurry vision) 。
- 閃光 ( flashes of light , photopsia ) :患者在視網膜無光線的刺激時仍在 周邊視野 見到閃光現象。這是因為玻璃體牽引視網膜所引起。
- 飛蚊 ( housefly ) :有些人周邊視野 ( peripheral vision ) 突然出現黑點 、黑影、蜘蛛絲 ( black dots, specks or streaks ) 在眼前飄動 ( a kind of cobweb effect of lots of little floaters ) ,這是因為視網膜破孔時產生微小玻璃體出血所引起,慢慢向中心擴散 ( slowly progresses towards the central vision ) ,可伴有 輕微 feeling of heaviness 。
因此,有上述各種症狀的人最好趕快找眼科醫師 ( Contact your GP immediately if you get any of these warning signs ) ,散瞳後徹底檢查眼底。 一旦視網膜剝離超過一定程度,會出現視野缺損、眼前有黑幕 (black curtain) 等 症狀。所幸, 80% 以上裂孔發生在周邊部,但 有時視網膜裂孔會發生於黃斑部位置,往往會有大範圍視網膜剝離而 產生色調或形體改變 ( suddenly appear curved , positive Amsler grid test ) 及 嚴重影響視力 ( central visual loss) ,且多半發生在老年人或有高度近視者。
視網膜剝離檢查包括:直接眼底鏡檢查(Direct Ophthalmoscopy,3-mirror scopy)、間接眼底鏡檢查(Indirect Ophthalmoscopy,90-diopter lens examination)。
滲出性視網膜剝離可採雷射光凝固、透鞏膜光凝、電燒、冷凍凝固 (cryopexy) 療法來治療 ,可促使視網膜裂孔周圍形成瘢痕組織以閉合裂孔 ( Laser or freezing treatment is used to scar the tissue around the retina, which creates a seal between the retina and the wall of the eye and closes up the tear or hole) 。
裂孔性或牽引性視網膜剝離 治療都是相當精密而複雜的手術,所以一定要找受過視網膜專科訓練的眼科醫師治療。早期發現而手術成功率在 75% 以上, 其處理方法有鞏膜扣壓術 (scleral buckling) 、玻璃體切除術 (vitrectomy) 、 氣體網膜固定術 (pneumatic retinopexy) , 使視網膜回復原位。
1 、 鞏膜扣帶術: 在眼後部的外部附著一條細小的扣帶,在眼壁上施加很小的力,使眼壁緊貼脫離的視網膜。 目的是減輕玻璃體對視網膜的牽引 。
(1) 鞏膜外加壓術: 扣帶 ( Bands) 多選擇 silicone rubber or sponge , 適用在較大的馬蹄形裂孔 (horseshoe tear) 、數目多的小圓形裂孔 (round holes) 和鋸齒緣離斷 (retinal dialysis)(S cleral buckling is the preferred way of re-attaching the retina if it has a tear or hole in it) 。
(2) 鞏膜環扣術:多用在 多發性視網膜裂孔超過兩個象限、視網膜脫離合并嚴重的增殖性玻璃體視網膜病變、巨大裂孔性視網膜脫離、視網膜脫離尚未發現裂孔。
2 、 玻璃體切除 術: 在玻璃體平坦部(pars plana)上切一個細小切口, 移除玻璃體以及結痂組織,隨後置換 gas bubble (SF 6 or C 3 F 8 gas) or Silicon oil (PDMS) 進 入 ,使視網膜緊貼眼壁 ( Vitrectomy works by removing the fluid from the inside of the eye and replacing it with either a gas or silicone bubble. This holds the retina in position from the inside ) 。 Silicon oil 常用在合併增殖性玻璃體視網膜病變者 ( Silicon oil is more commonly used in cases associated with proliferative vitreo-retinopathy (PVR)) 。
3 、 氣體網膜固定術 ( Pneumatic retinopexy ) : 將 可膨脹 氣體或矽油充填到玻璃體腔 ,幾天內氣泡慢慢膨脹,使視網膜重新附著在眼壁 ( A bubble of expandable gas is injected.Over several days, the gas bubble expands, eventually causing the retina to reattach itself to the wall of the eye) ,此法 適用糖尿病玻璃體視網膜病變及黃斑部裂 孔。
手術後有 15% 有時需要 2 次以上手術 ( 85 percent of cases will be successfully treated with one operation with the remaining 15 percent requiring 2 or more operations ) 。手術後 2~4 週內要避免劇烈運動,如 Bungee jumping 、 Skydiving 、 Defecation 、 Space travel 、 Weightlifting 、 Roller coasters ,也 避免過度疲勞及 不要提重物。一般周邊部視網膜剝離者,有 50% 以上可以回復原先視力。
<97-1-10> 下列有關背景型糖尿病視網膜病變( background diabetic retinopathy; BDR )的敘述,何者錯誤?
- 視網膜病變局限於視網膜內( intraretinal )
- 微血管瘤( microaneurysms )是其早期視網膜病變之特徵
- 黃色視網膜滲出物( hard exudates )亦是其視網膜病變之特徵
- 需要積極視網膜雷射治療( laser photocoagulation )以防止惡化
<97-2-9> 如眼底視網膜照片所示,此位患者最可能之診斷為何?
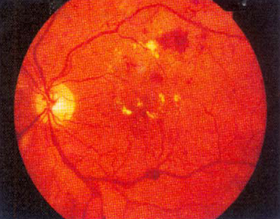
- 糖尿病視網膜病變
- 急性視網膜中心動脈阻塞
- 急性視網膜中心靜脈阻塞
- 早產兒視網膜病變
<97-2-10> 承上題,此位患者最適當之處置為何?
- 眼球按摩並降低眼壓
- 積極控制血糖及眼科門診追蹤
- 泛視網膜雷射治療( panretinal laser photocoagulation; PRP )
- 玻璃體切除術( vitrectomy )
<98-2-12> 後眼部玻璃體切除術( vitrectomy )一般是經由何處進入眼內?
- 玻璃體基底部( vitreous base )
- 鋸齒緣( ora serrata )
- 皺摺部( pars plicata )
- 平坦部( pars plana )
<99-2-10> 下列何者不是門診檢查視網膜的主要方法?
- 間接眼底鏡檢( indirect ophthalmoscopy )
- 直接眼底鏡檢( direct ophthalmoscopy )
- 間接細隙燈鏡檢( indirect slit-lamp biomicroscopy )
- 視網膜鏡檢( retinoscopy )
<99-2-12> 下列何種周邊視網膜變性與視網膜剝離關係最密切?
- 囊狀視網膜變性( cystoid degeneration )
- 格子狀變性( lattice degeneration )
- 萎縮性視網膜裂孔( atrophic retinal hole )
- 卵石狀視網膜變性( paving stone degeneration )
<99-2-14> 下列有關增殖型糖尿病視網膜病變( proliferative diabetic retinopathy, PDR )之敘述,何者錯誤?
- 增殖型視網膜病變主要發生於視網膜下腔( subretinal space )
- 視網膜新生血管( neovascularization )是此病變之特徵
- 可造成玻璃體出血( vitreous hemorrhage )
- 可導致牽引型視網膜剝離( tractional retinal detachment )